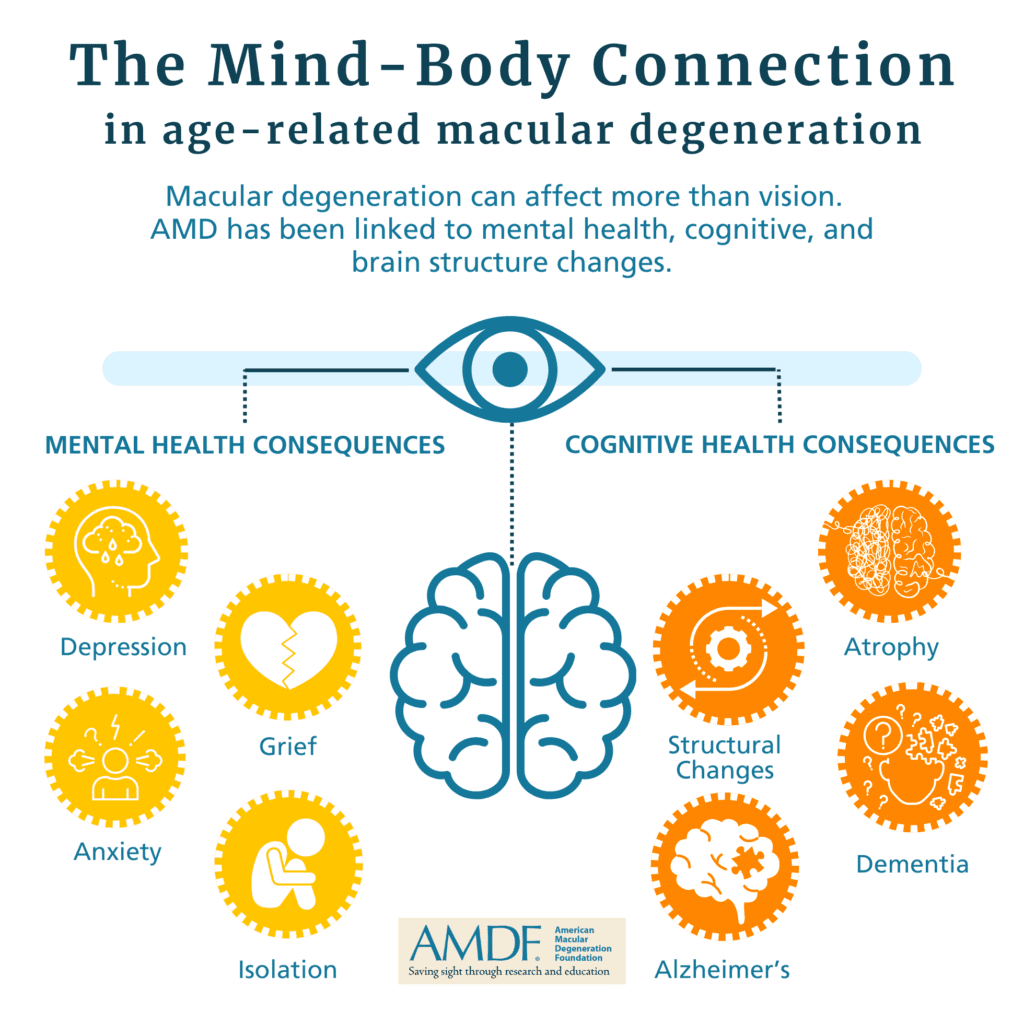
Much is discussed about the effect of macular degeneration on the eyes and vision, and even daily living, but macular degeneration and vision loss also have profound effects on the well-being of the mind and brain.
From initial diagnosis to dealing with vision loss, or the fear of vision loss, each stage of disease progression can impact emotional well-being. And the physical structure of the brain is impacted by both the disease pathogenesis as well as diminished visual input and its impact on activities and social stimulation.
Macular Degeneration and Depression
Research shows that people with AMD are more likely to experience depression compared to those without the condition (Dawson et al., 2014). As your central vision gradually declines, you might start to feel anxious about the future and frustrated with daily tasks that become harder to manage. These feelings can sometimes lead to depression.
If you have advanced AMD, you might find the emotional impact even more profound. Significant vision loss can make it tough to do things you love and maintain your independence. This can lead to feelings of isolation and loneliness, which are common triggers for depression (Cimarolli et al., 2015). It’s important to recognize these feelings and seek support to help you navigate this tough time.
Your vision affects your overall mental health significantly. As your eyesight worsens, the risk of depression increases. It’s crucial to address both the physical and emotional aspects of AMD in your treatment plan. A holistic approach, including mental health support and vision rehabilitation, can help you adapt to your vision changes and improve your overall quality of life (Fonteh et al., 2022).
Macular Degeneration and Anxiety
Macular degeneration can also cause anxiety. The fear and uncertainty that come with progressive vision loss can be overwhelming. Research shows that people with AMD often experience high levels of anxiety, especially as the condition progresses (Dawson et al., 2014). You might constantly worry about how your vision loss will affect your daily life and your ability to stay independent, which can lead to persistent anxiety.
Advanced AMD can also make you anxious about safety and mobility. You might fear falling or struggle to navigate even familiar environments, which can heighten feelings of vulnerability and stress (Popescu et al., 2012). This anxiety can lead to avoiding social situations and further isolation, adding to the emotional burden of AMD.
To manage anxiety, it’s important to have a comprehensive care plan that includes both physical and emotional support. Rehabilitation programs, mental health counseling, and support groups can provide you with coping strategies and emotional support. By addressing these concerns, you can maintain a higher quality of life despite the challenges of AMD (Fonteh et al., 2022).
Remember, you’re not alone. Seeking support from healthcare providers, family, and friends can make a significant difference in managing the emotional challenges of AMD. By addressing both your physical and emotional needs, you can lead a fulfilling life despite your diagnosis.
Macular Degeneration and Grief
There is little in the formal literature about grief and macular degeneration, but we know from anecdotal reports from both patients and those working with them in the field that grief is part of the process of vision loss. Ann Wagner, PhD, LP, ABPP, Board Certified Clinical Psychologist, who herself has direct experience with progressive vision loss, wrote the following for a recent piece in our print newsletter, In the Spotlight:
“Progressive vision loss is not something one can grieve once and then be done with it. Grief follows grief. People with progressive vision loss or other disabilities experience a complex grief that reasserts itself in response to each decline in daily functioning. Some losses of function may involve activities a person decides they can get along without. Others, however, involve activities that a person highly values. Their loss requires not only grief but expenditures of time, energy, money, technology, rehab services, etc., to learn new ways to move forward.”
Macular Degeneration and Isolation
For some people, central vision loss becomes severe enough that it becomes difficult to recognize faces and limits mobility and outings. This can naturally lead to social isolation, which in turn can exacerbate depression.
Macular Degeneration and Structural Changes to the Brain
Age-related macular degeneration (AMD) not only affects your vision but can also lead to structural changes in your brain.1 When you lose central vision due to AMD, the part of your brain responsible for processing visual information from the macula (the central part of the retina) receives less input. This lack of stimulation can cause the neurons in the visual cortex to reorganize and start responding to input from other parts of the retina. This phenomenon is known as neural plasticity.
In simpler terms, your brain tries to adapt to the loss of vision by “rewiring” itself to use other parts of your retina for visual tasks. For example, if you lose vision in the central part of your visual field, your brain might start using a different area of your retina to help you see. This reorganization can help you compensate for some of the vision loss, but it also highlights the brain’s incredible ability to adapt to changes in sensory input.
It’s fascinating to see how interconnected our brain and eyes are, and how our brain can adjust to maintain functionality even when faced with challenges like AMD.
Macular Degeneration and Brain Atrophy
Age-related macular degeneration (AMD) has been linked to brain atrophy, which is the loss of neurons and the connections between them. A study by researchers at Duke University2 found that people with AMD experience more rapid deterioration of brain tracts over time compared to those with healthy eyes. This means that the brain regions responsible for processing visual information may shrink or lose function more quickly in individuals with AMD.
The exact mechanisms behind this link are still being studied, but it’s believed that the same risk factors that contribute to AMD, such as aging and inflammation, may also play a role in brain atrophy. Additionally, the reduced visual input from the damaged macula might lead to changes in the brain’s structure and function.
Macular Degeneration and Cognitive Decline
Age-related macular degeneration (AMD) has been linked to cognitive decline, including an increased risk of dementia3. Studies have shown that individuals with AMD are more likely to experience cognitive decline and dementia compared to those without AMD. The exact mechanisms behind this link are still being studied, but it’s believed that reduced visual input from the damaged macula may lead to changes in the brain’s structure and function.
Cognitive decline refers to the gradual loss of cognitive functions such as memory, attention, and reasoning. It can range from mild cognitive impairment (MCI), which involves slight but noticeable changes in cognitive abilities, to more severe forms like dementia and Alzheimer’s disease4.
Dementia is a broad term for conditions characterized by a decline in cognitive function that interferes with daily life. Alzheimer’s disease is the most common cause of dementia, accounting for 60-80% of cases. It’s caused by abnormal protein build-up in the brain, leading to cell death and damage to connections between neurons.
Disclaimer: This information is for general knowledge and does not constitute medical advice. The provided sources are examples and may not be exhaustive. If you or someone you know is experiencing mental health or cognitive challenges related to AMD, please consult with a medical professional.
This information is designed to be a starting point for your research. You should always consult with a qualified healthcare professional for any health concerns.
References
- What drives brain changes in macular degeneration? https://news.mit.edu/2009/macular-degen-0303 ↩︎
- Stout JA, Mahzarnia A, Dai R, et al. Accelerated Brain Atrophy, Microstructural Decline and Connectopathy in Age-Related Macular Degeneration. Biomedicines. 2024;12(1):147. Published 2024 Jan 10. doi:10.3390/biomedicines12010147 ↩︎
- Eye Diseases Linked to a Higher Risk of Dementia. https://www.health.harvard.edu/mind-and-mood/eye-diseases-linked-to-a-higher-risk-of-dementia ↩︎
- Alzheimer’s Disease, Dementia, and the Eye. https://www.aao.org/eye-health/diseases/alzheimers-disease-dementia-eye ↩︎

